Spinal Infections – Understanding Spondylodiscitis
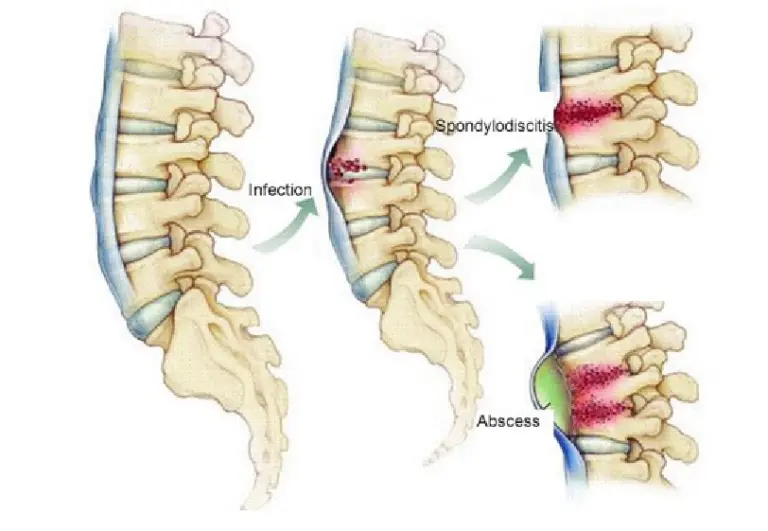
Spine infections often begin at the disc level and gradually involve the neighboring spinal bones, a condition known as spondylodiscitis. The most common culprits behind spondylodiscitis are TB (Tuberculosis), bacterial, and fungal infections, in that order.
TB Spondylodiscitis
In India, TB infection of the spine is prevalent and can affect people of any age, including those in good health, without gender preference. Many individuals carry TB bacteria in their respiratory system, which can become active when their immune system weakens. The TB bacteria can enter the bloodstream and take hold in the spinal disc and vertebrae, leading to pus formation and damage.
Symptoms
The symptoms usually persist for months and include neck or back pain, a rise in temperature in the evenings, weight loss, loss of appetite, night pain, and potential neurological symptoms such as sensory loss and weakness. Spinal deformities like kyphosis or pressure on the spinal cord (canal stenosis) due to pus and bone damage can also occur.
Management & Treatment
Diagnosis involves blood tests and imaging like X-rays, MRI, and CT scans to assess spinal stability. In cases of a stable spine, the primary treatment is anti-tubercular therapy (ATT) for 12-18 months. Surgery may be necessary if the spine is unstable. Confirming the TB infection through a biopsy and identifying the drug susceptibility of the TB bacteria is crucial for treatment.
Pyogenic Spondylodiscitis
In contrast to TB, pyogenic spondylodiscitis is more common in the elderly and those with compromised immune systems, uncontrolled diabetes, renal dialysis, liver failure, or following procedures including spine surgeries. Bacteria enter the bloodstream due to weakened immunity and primarily attack the spinal disc, causing damage through pus formation.
Symptoms
Pyogenic infections present acutely with symptoms lasting only a few days. These individuals typically experience severe back pain, high-grade fever, and often find themselves bedridden due to their poor overall health
Management & Treatment
Blood tests in pyogenic infections often show significant abnormalities, such as low hemoglobin, elevated WBC counts (especially neutrophils), increased ESR, CRP, and positive bacterial growth in blood or urine tests. Biopsy is crucial for identifying the type of bacteria. Treatment primarily involves IV antibiotics for about 6 weeks. Surgery is usually not required, as these infections typically respond well to antibiotics. However, surgery may be considered to reduce bacterial load and facilitate early mobilization in some cases.
Why Dr. Ramachandran
Many surgeons often follow empirical treatment with ATT or antibiotics, even in recent times. This approach can lead to delays in diagnosis or incorrect treatment, worsening the infection.
Dr. Ramachandran practices evidence-based medicine by conducting a CT-guided biopsy and initiating ATT or antibiotics based on the biopsy report. This approach aims for early recovery and successful eradication of the infection from the body, providing patients with a well-informed and effective treatment plan.
